ATM Theory: Your Joint Pain May Actually be Muscle Pain

ATM = Always Think Muscles. When you’re trying to get to the root of your joint pain, don’t forget to assess muscle function around the joint. Chances are, this is where your challenge lies, and that functional training can help you overcome it.
Table of Contents
- Understanding Joint Pain
- Why the Orthopedic Theory of Joint Pain is Wrong
- Your Labrum, Meniscus, and Intervertebral Discs are Just Not That Important
- Why Most Joint Pain is Really Muscle Pain
- Joint Pain and Post-Workout Muscle Soreness
- Joint Pain and Pushing Muscles Beyond Their Limits
- Joint Pain and Consistent Muscle Pain
- 3 Ways to Think About and Resolve Joint Pain
Here’s a controversial statement: joint pain is really almost always muscle pain.
I don’t have any placebo-controlled studies to back up my theories on this, but I do have thousands of hours I've personally spent with clients since 2007. Plus, the Upright Health team, past and present, has thousands more hours of experience with their clients. This is what we have observed about joint pain and functional training.

Joint pain in the wrist, by Towfiqu Barbhuiya, via Unsplash
Understanding Joint Pain
Let's start by defining some key concepts.
A joint is where two bones meet. It's not one specific object. It's a point in space where multiple things happen.
For example, this is your knee joint (below). It's where your femur (thigh bone), tibia (shin bone), and patella (knee cap) meet.
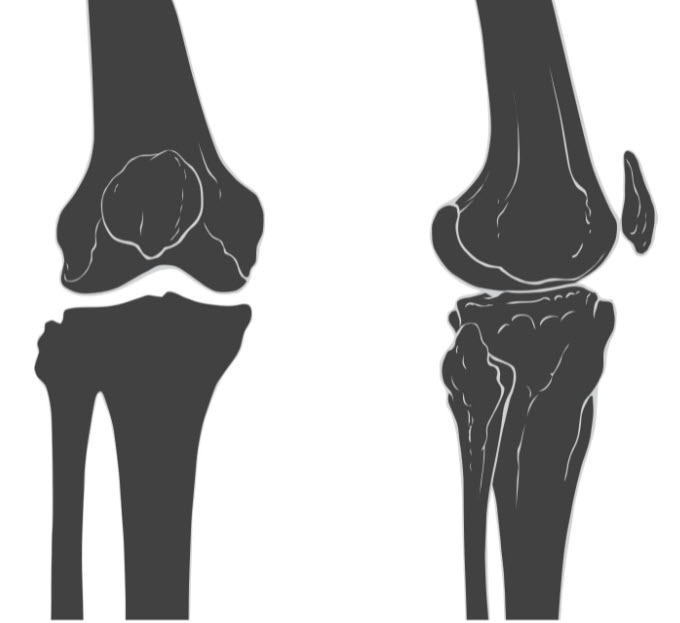
Knee joint illustration, by Patrick J. Lynch, CC BY 2.5, via Wikimedia Commons
Below is your shoulder joint. It's where your humerus (arm bone), scapula (shoulder blade bone), and clavicle (collar bone) meet.
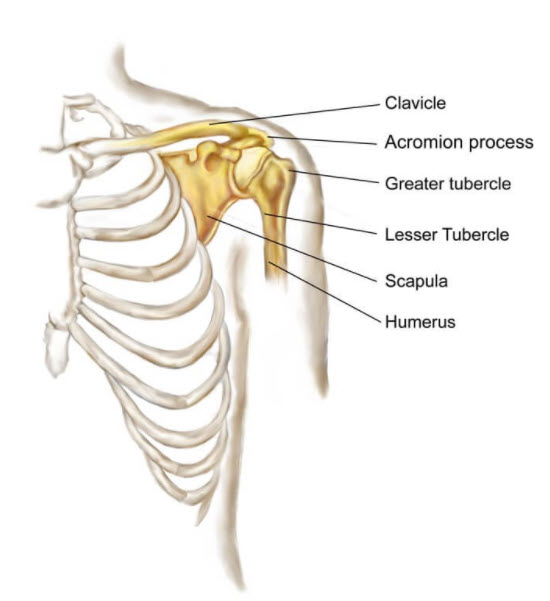
Around the joint space, you'll see things like tendons and ligaments. A tendon is tissue that joins muscle to bone. A tendon is not separate from a muscle. It has a different texture and toughness than the rest of the muscle and has thus earned a different label.
Ligaments attach bones to one another. The ACL (anterior cruciate ligament) attaches the thigh bone to the shin bone, for example. Ligaments are super tough (but obviously can be snapped under stress).

Anterior cruciate ligament tear illustration, by BruceBlaus, CC BY-SA 4.0, via Wikimedia Commons
Muscles, tendons, and ligaments provide stability to joints. These are sometimes called "soft tissue" because they are not as hard and rigid as bone. Without these soft tissues, nothing holds the bones in relation to each other (or in relation to the floor!).
The only reason you can keep your head up is because you have muscles, tendons, and ligaments working to keep your skeleton arranged vertically throughout the day.
There are also structures inside joint spaces. You find things like cartilage and cartilaginous padding (called labrums, discs, or menisci depending on where they are in your body).
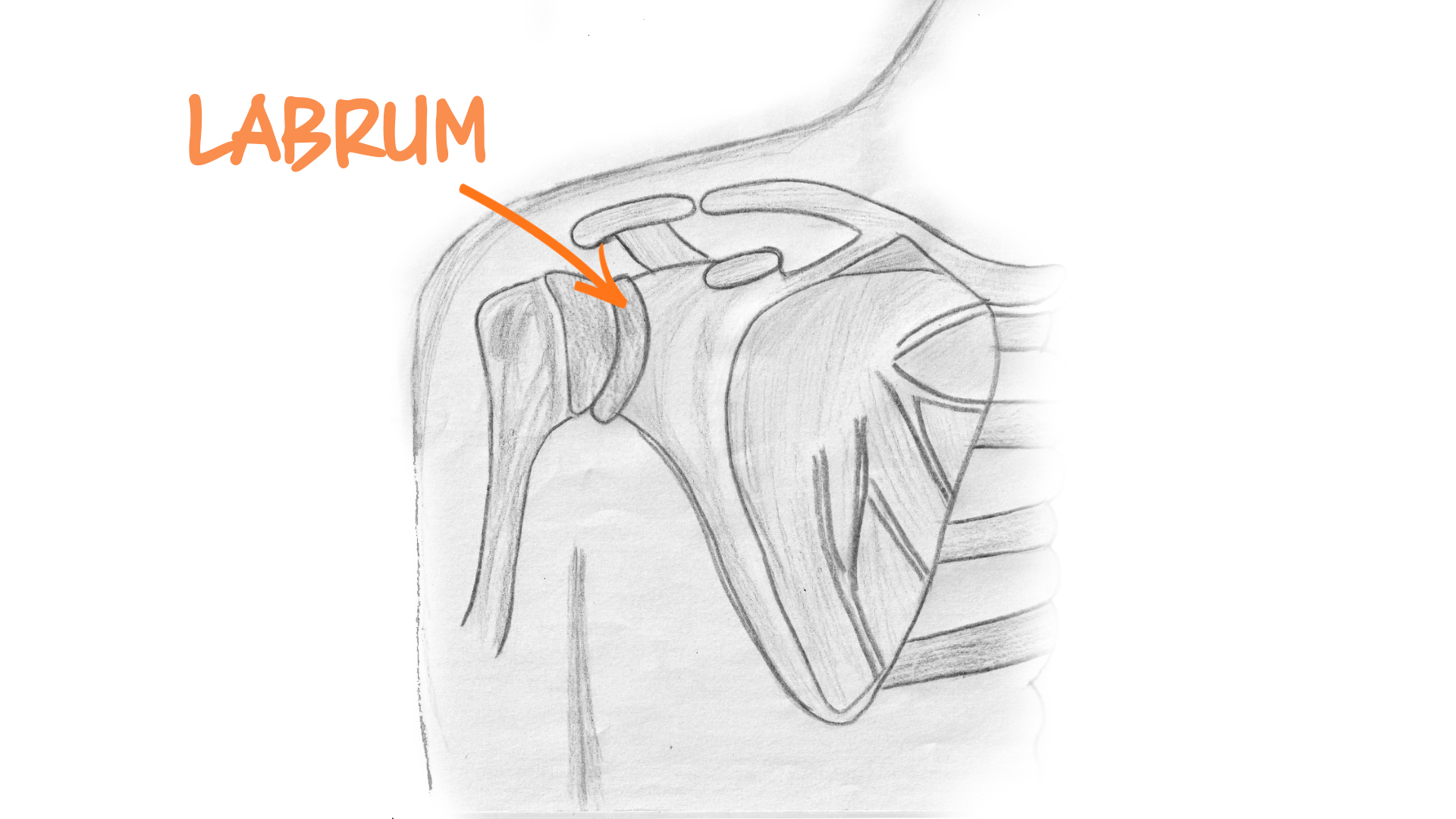
Shoulder Labrum Tear Illustration
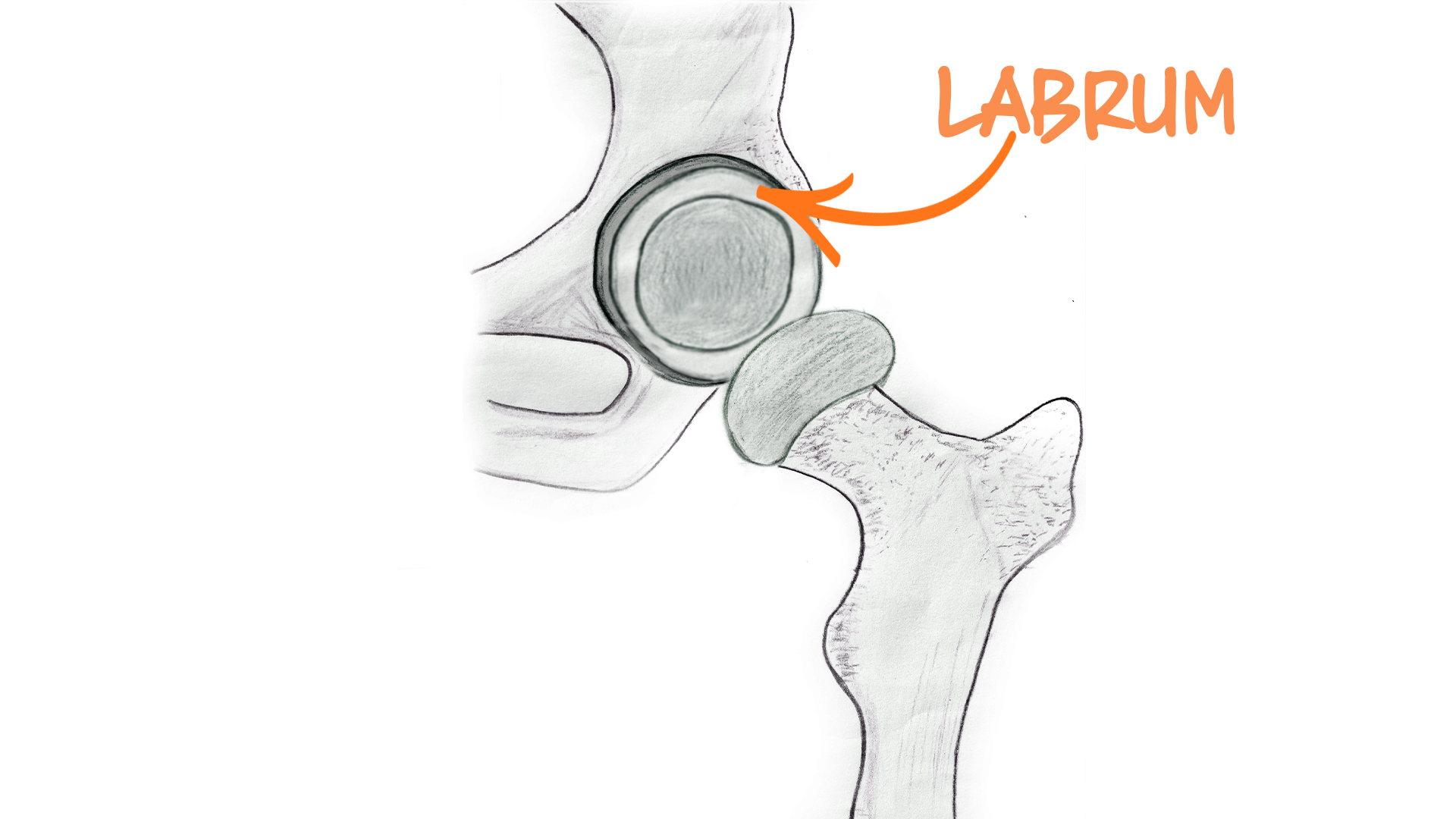
Hip Labrum Tear Illustration
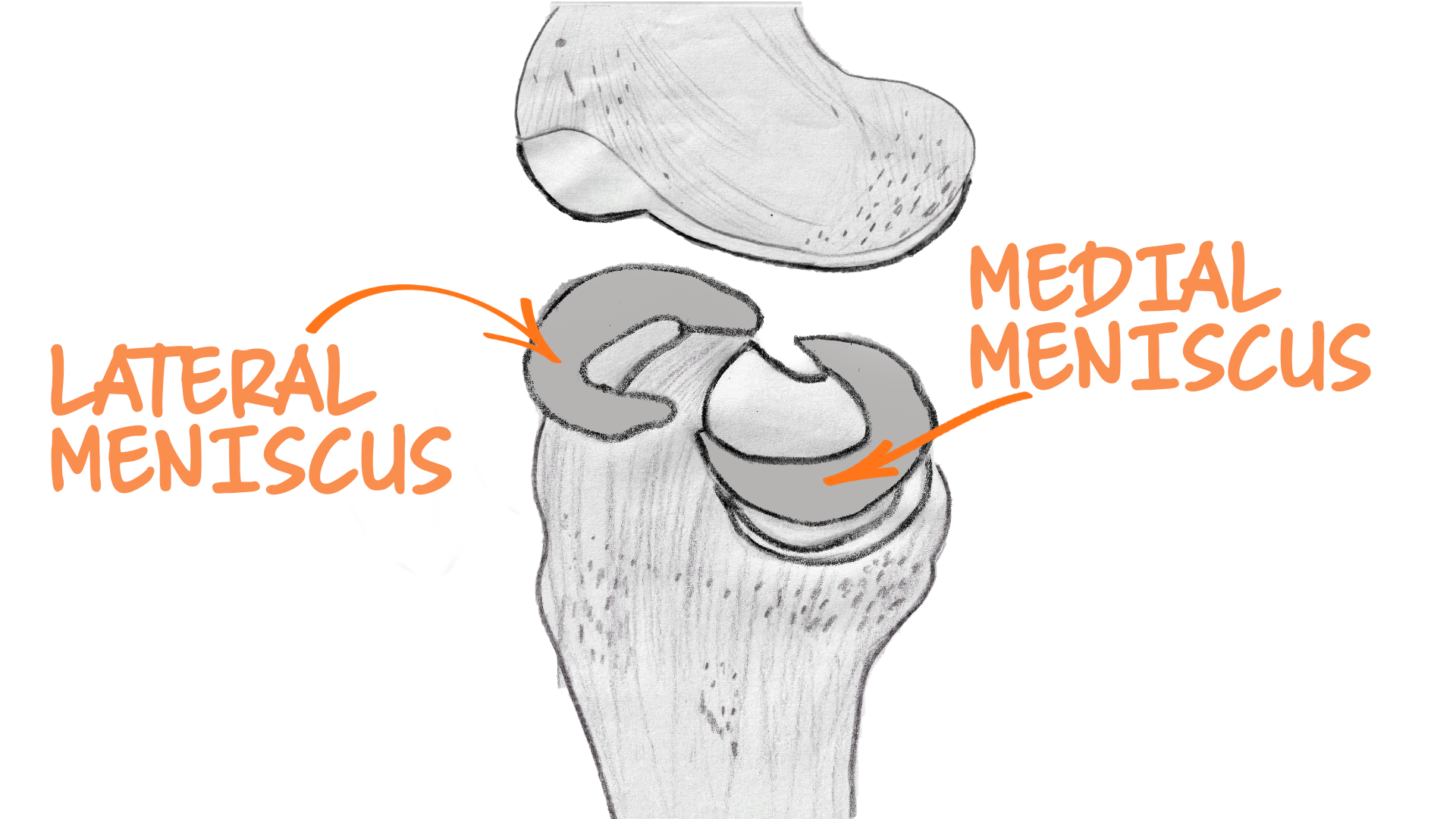
Lateral and medial meniscus and cartilage illustrations,
Current conventional medical theories say that these structures act as shock absorbers and friction mitigators. We'll just call them "cushions" collectively from here on.
Doctors claim that these cushions wear out due to a number of factors. When cushions wear out, you allegedly get pain in the joint space because bones now collide.
See also: The Secret History of Joint Pain
Why the Orthopedic Theory of Joint Pain is Wrong
The conventional orthopedic model of joint pain, in which bone-one-bone collisions cause discomfort, is full of errors, in my opinion.
Here’s why: When you run or jump, you have a meniscus in the knee joint that prevents the hard bones from smashing into each other, thus saving them from damage.
When you're running, you also bend and straighten your knees over and over again. In this case, cartilage and meniscus prevent the hard bones from rubbing directly together. This reduces the damaging effects of friction.
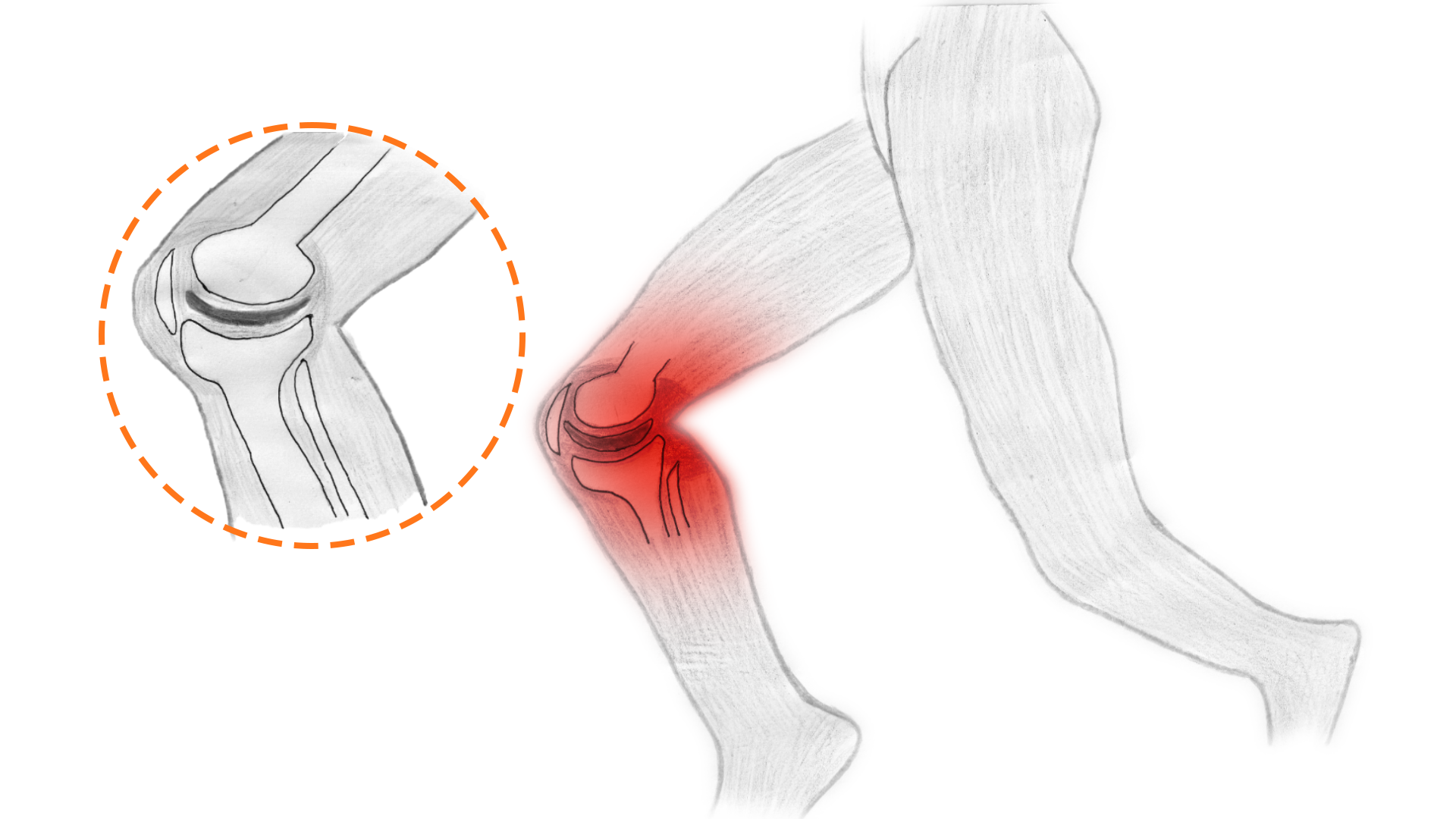
Medical illustration of knee impact from running
When these cushions are used too often or too hard, they allegedly "wear out" and no longer function well. The bones then touch one another and you experience pain - inside, and potentially around, the joint.
Once this bone-on-bone contact occurs, the joint can no longer be used pain-free and, according to orthopedic theory, must be surgically fixed or replaced.
Orthopedic surgeons may also tell you that torn cushions need to be fixed. But labrum tears and meniscus tears are highly prevalent in people with no symptoms!
With hip labrum tears, there is no correlation with pain or other symptoms. With knee arthritis and meniscus tears, there is no correlation with pain or other symptoms (a detailed 2020 MRI study showed meniscus tears are highly prevalent in the asymptomatic population). With shoulder labral tears, there is no correlation with pain or other symptoms.
See also: Hip Labral Tears: What You Need to Know and What Your Doctor Won’t Tell You
This means that there is no observable causative link between labral tears, meniscal tears, or bone deterioration and pain. And we can't even be sure if one specific accident or incident creates a tear in a labrum or meniscus.
It's impractical to even attempt to investigate this. To track when a tear occurs, you'd need to be doing scans every day—perhaps multiple times a day.
To summarize, in the conventional orthopedic medicine model of joint pain, the major causes of joint pain are cushions wearing out and bones coming in contact with other bones.
Based on this theory of the human body, doctors will tell you that you should NOT run very much or for very long in your life. The padding in your knee joints (or any joint) has a limited life span. The more movement you force it to cope with, the faster it wears out.
The Normalcy of Bone Abnormalities
In addition, doctors have claimed that specific shape "abnormalities" result in joint pain.
Misshapen bones allegedly collide with other bones as a result of the bone shapes. These misshapen bones allegedly smash and destroy the cushions within joints. This perspective underpins theories for hip and shoulder pain (hip impingement and shoulder impingement).
But these theories are wrong, and researchers have known it for decades.
Meme of fish with 'something smells fishy'
Bone-on-bone contact doesn't cause pain.
First of all, multiple studies have shown that bone-on-bone arthritis in an X-ray of your knees, hips, spine, or any other joint, has zero correlation to pain or function. And conversely, the alleged damage and deterioration you see in medical images does not correlate at all to pain or range of motion.
If bone-on-bone contact does not correlate with pain or loss of range of motion, the orthopedic theory of joint pain falls apart.
But there's more to the story, and it involves those little pieces of cushioning in your joints.
See also: How Shifting Your Perspective on Chronic Pain Can Help You Heal
Your Labra, Menisci, and Intervertebral Discs are Just Not That Important
Sometimes parts of a cushion remain between bones in a joint. Surgeons say that damaged cushions themselves generate pain. Without rhyme or reason, orthopedic surgeons often say these cushions need to be removed.
Then someone discovered that this procedure made patients worse off (oops!). Instead of doing some deep soul-searching and scientific investigation, the orthopedic surgery profession decided that cutting away a piece of torn meniscus or trying to repair it was better.
It's important to remember this story: Surgeons operate on joints with undue confidence, and once they've changed your body, it can't be undone.
The theory that labra, discs, and menisci are our primary friction reducers and shock absorbers is garbage.
Labra, menisci, and intervertebral discs do probably absorb some impact, but to think that preventing joint pain relies on those little structures tests the limits of credulity.
In fact, thinking of labra or menisci as "shock absorbers" makes about as much sense as using a newspaper to cushion an egg that you drop to the floor.
Think about this: Hip labra are 2-3mm thick.
The knee menisci are about 3-5mm thick.
To get a sense of that, a penny is 1mm thick. So your little hip cushions are about two or three pennies thick. And your knee menisci can be three to five pennies thick.
That's not thick.
And unless the cushions are made of some kind of incredible space-age, impact-dispersing substance, they’re not enough to absorb the impacts we regularly subject our bodies to.
We could probably do some sophisticated mathematical modeling of all these tissues and figure out what forces these things can withstand and mitigate… but since we don't have a research lab at our disposal and such research would be ripe for error and misunderstanding, let's just take a cheap and logical look at the issue. We can observe the real world to understand the reality around these alleged cushions.
For example, children are able to participate in sports like gymnastics, soccer, hockey, karate, and skiing. All of these activities will result in many thousands of repetitions of high impact on the hip labra and the knee menisci. These children do not immediately decay into piles of pain. They don't even start hurting within one year of beginning impact sports. How does a 2-5 mm cushion handle such repetitive loading? Shouldn't it be demolished within a year?
See also: Joint Injections for Pain – Do Risks Outweigh Benefits?

Man Jumping Photo by William Rouse on Unsplash
Take another example: A 160-pound adult who can land high drops and massive falls multiple times as a part of his profession.
Damien Walters is an adult who grew up doing gymnastics. He can perform incredible stunts that would be literally impossible if impact absorption were dependent on a 2-3 mm piece of tissue in his hips and knees. And if a human's thin little cushions were in fact as fragile as orthopedic surgeons claim, his little shock absorbers would be absolutely shredded and compressed to bits (seriously, watch what he can do).
Through a classic orthopedic lens, Walters should have been confined to a wheelchair by the time he was 20 years old. But, clearly, he wasn't.
Following this thought experiment, let's acknowledge this: Not all children and not all adults can absorb impact well initially, but can teach their bodies to get more adept at it.
This is important.
If we see that human beings can improve their ability to absorb impact, then we have evidence that it is a skill that is not tied to the condition of a tiny 3 mm cushion that degrades over time. It indicates that muscle firing patterns and timing are far, far more important.
The labra or menisci are not the limiters of physical capacity.
All this talk about the cushions wearing out stems from outdated ideas from the 19th century. There's actually evidence that our cartilage doesn't wear out due to usage. It decays and declines due to lack of usage! (Read this article on creaky knees and this one on cartilage damage and exercise.)
The idea that your knee, hip, shoulder, or spinal joints are bounded by a finite number of uses before wearing out sounds plausible. It's an analogy that mirrors what we see with human-made tools like chairs, hammers, car tires, and more.
But human joints are not the same as human-made tools. Human joints are biological. They respond dynamically to usage. In fact, usage seems to be necessary to prevent total breakdown.
I have watched a two-year-old learn how to absorb impact. My son practiced jumping off the couch many times before he was able to do it with confidence. If he develops as a normal human, his body will be able to handle larger drops and jumps without any issue for decades to come. With every passing month, the heights from which he is comfortable jumping increase.

A man practices flips on the beach
Likewise, I've watched 40- and 50-year-olds learn how to land jumps properly after years of ineptitude. Their first attempts were clumsy, stiff, and awkward. Their knees may have been sore. But, over time, they learned how to fire muscles at the right time and at the right length to attenuate the forces pain-free.
And this brings me to my main point: Anyone who has any experience absorbing impact in any activity has direct experience with the fact that impact absorption is a product of muscle strength and coordination, not of the thin strips of cartilage between bones.
See also: What Absorbs Impact?
Why Most Joint Pain is Really Muscle Pain
We can see that the modern medical understanding of joint pain is based on flimsy ideas.
Surgeons of the late 19th and early 20th centuries were looking for structural things to fix. They tried to blame structural abnormalities for every bit of pain you experience. But modern science keeps showing that this just doesn't hold water.
So where should we put our attention?
We need to look at muscle function and the muscles themselves.
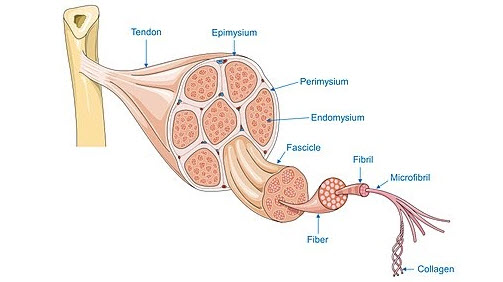
Muscles are responsible for movement. They are responsible for how we hold our bodies. They regularly give us pain signals. We know that using muscles in particular ways can cause particular kinds of pain and discomfort.
There is no question that muscle over-usage and under-usage can cause pain. There is no question that under-stretching and overstretching muscles can cause pain.
When you wonder where your joint pain is coming from, I have a productive strategy that I abbreviate as ATM: Always Think Muscles.
Under the ATM theory, you identify what muscles are hurting and what factors are contributing to those muscles hurting (e.g. joint muscle imbalances or plain muscle dysfunction).
I don't get caught up in orthopedic ideas like misshapen bones or torn labra or arthritis.
While many orthopedic surgeons recommend protocols for rest, ice, injections, pills, and surgery (what I call RIIPS) to address joint pain, ATM is the better choice. Even when the pain feels like it's in the joint, I prioritize investigating the muscles around the joint.
Of course, joint pain could be caused by rare exceptions like cancer and infectious diseases, but those are the outliers. It's a great idea to rule those things out medically, while also remembering to ignore the orthopedic hoodoo about damage and misshapen bones.
Keep on ATM-ing.
See also: How Shifting Your Perspective on Chronic Pain Can Help You Heal
By following the Always Think Muscles (ATM) philosophy, you accomplish three major victories:
- You maintain a sense of agency and responsibility. There is nothing as disempowering as believing that your body is defective and that you are powerless to improve it.
- You learn to listen to and work with your body. Many people have been trained from a young age to ignore subtle (and not-so-subtle) signals of physical discomfort.
Ignoring your body can be helpful in short bouts to accomplish important goals. But in the long-term, it leads to bodies that simply don't move well due to chronic misuse.
It's similar to sleep deprivation. Can you stay up all night to finish that important paper for school? Yes. Will it drastically harm you? No. But if you did that every night for a few years, you would definitely be harming your body.
- You protect the body from unnecessary harm. Injections and surgeries are not risk-free undertakings. Surgeries are invasive and permanent assaults on your body.
Before the advent of anesthesia and antibiotics, humans were loath to cut through the skin to fix anything. Doing so would surely invite death via systemic shock or infection.
Medical technology has come a long way, and we can now keep people alive, even after severe traumas like motorcycle accidents, gunshot wounds, and explosions. But this doesn’t mean we should blindly march into surgeries thinking they are risk-free, especially when modern science shows they are often risky and without benefit beyond placebo.
Highly popular surgeries like hip replacements have infection rates that hover around 1 percent. While this sounds like a small risk, the results of a hip replacement infection can be catastrophic for something that is based on a questionable understanding of the human body.
In short, it's best to ALWAYS THINK MUSCLES.
See also: How to Fix Muscle Dysfunction and Muscle Imbalances
Let's look at common examples of muscle pain and see how they can contribute to our understanding of joint pain.
Joint Pain and Post-Workout Muscle Soreness
There are theories about what causes muscle soreness on a cellular level. Micro-tears from strong, repetitive muscle contractions are commonly blamed for muscle soreness. Read this article for some theories and related research.
Another potential piece of the painful muscle puzzle gets deeper into neuroscience, so I won't dwell on it. If you're a neuroscience nerd, I'd appreciate some insight into this. I wonder if the shortened post-workout state causes a proprioceptive mismatch — a phenomenon believed to cause phantom limb pain.
In any case, we needn't get lost in the minutiae. We need to have a practical understanding, and let the research scientists wrestle with the nuts and bolts.
In the case of post-workout muscle soreness, the simplest and most productive interpretation is that soreness is a signal that the muscle has low overall work capacity relative to the demands being placed on it.
This would explain why stretching and massage can often relieve post-workout soreness. It would explain why you might get sharp pains from seemingly small movements. It would explain why some weak muscles could feel painful on a regular basis despite almost no usage.
For example, let's say I did a lot of shoulder exercises two days ago. Today my shoulders are sore when I sit at the computer and move my arm to grab the mouse.
My shoulder muscles are at a low level of strength relative to all of these simple tasks. The pain is telling me to be careful. Is it a sign of damage? On a cellular level, it might be. Are the muscles in a shortened state? Sure. Could there be a mismatch between what the brain expects and what the body can do? Sure. The important thing to note is that this is a temporary situation.
We experience the low-level warning of soreness so that we do not attempt to repeat an intensity of activity that would injure us in our currently weakened state. The soreness just says "We can't quite do this particular activity without your careful attention right now. And, you know, maybe we should just take it a little easy today, huh?"
How many weekend warriors do you know who have ignored soreness after an intense workout and then tried to do another super intense workout? Was anyone surprised when they promptly injured themselves?
The takeaway is simple: When muscles are too weak to meet the demands of a specific movement, they tell us.
Joint Pain and Pushing Muscles Beyond Their Limits
Much like with post-workout muscle soreness, pinching pain tells us that the current aggregate strength of our muscles is at, or near, its maximum.
A common example is pain and pinching in the groin muscles. People often complain of groin discomfort when getting into specific positions. Maybe it's going into a deep squat. Maybe it's spreading the feet and legs wide. Maybe it's pulling the feet in toward the midline. It could be a dull or sharp pain. No amount of stretching or massage makes it go away.
The medical model of joint pain conditions us to think, "Well, this must be a torn muscle or bad cartilage or a damaged joint." But this completely skips a less catastrophic, and more helpful interpretation.
In reality, we have dysfunctional muscles that struggle to meet current strength and length demands.
We need to train the muscles gradually to meet the demands we place on them. The simplest way to do that is to keep practicing motions that engage the neural pathways that contract the muscle. More simply, you need to strengthen and lengthen.
For example, one day you realize that you can't bend at the hips and touch your toes. You can barely reach past your knees. The backs of your thighs (hamstrings) feel sharp, stiff, and tight. That's not a sign of damage or disease. It's a sign of dysfunctional muscles. You teach the muscles to lengthen (i.e. stretch) as well as strengthen (i.e. contract) in those lengthened positions. Over time, you can touch your toes!
For people who are already super flexible and bendy, the process is a little different. It entails strengthening muscles in shortened and lengthened positions.
For example, some yoga practitioners are notoriously too flexible and still have the feeling of tight muscles or pinching and jamming in their groins and outer hips. Stretching muscles that are already able to lengthen is pointless. Building strength in the hip muscles in various positions and angles is the key to relieving the sense of tightness.
In short, you can build strength at every length.
See also: How Do You Relax Tight Muscles?
Joint Pain and Consistent Muscle Pain
Now, let's put this all together and look at the final case that confounds people most often— muscular pain even when they haven’t worked out or are not actively using the muscle
The answer is that whether you are consciously trying to use a muscle or not, it's trying to do something. If you exist in gravity, you require muscle activity to maintain physical integrity. It’s a matter of survival. Your muscles cannot just allow a bone to drop out of place willy-nilly. Without your muscles, you would be a sack of bones and blood stuck on the floor.
If the aggregate strength of any muscle is not enough to meet the demands of sitting and standing around, your body should and will tell you so.
Examples of this kind of muscle-weakness feedback abound.
If you sit for more than 80 percent of your waking hours, you may constantly feel like your butt and groin are tight or tense. You could also feel fine while sitting, but sense something sharp in the joint when standing.
Listen to my podcast on the secret history of joint pain.

Woman sitting at desk touching her back in pain
This is clearly not a situation in which your muscles are overworked and overtrained and thus sore. (And it’s clearly not a situation in which your bones are being damaged by excess loads.)
Think about this: People confined to their beds for days, weeks, or months don’t feel like they’re relaxed and comfortable the whole time. They get sore and achy in the muscles and joints (also really still their muscles 😄). Left long enough, they get bed sores.
Think back to the last time you said to yourself, I’ll just lie in bed all day and relax!
How much shifting, turning, and rolling did you do? If you’re like most human beings, you physically can’t just lie there, locked into one position all day. If you did (because you were mesmerized by Twitter), when you finally did start to move, your body probably felt sore in a few particular spots—likely your back, hips, or neck.
Do you know what would’ve prevented that soreness and stiffness? Movement.
Movement requires muscle contraction! Blood flow requires muscle contraction!
Another example is the 55-year-old man who’s been working at a desk for the last 30 years. He plays tennis once a week when the weather’s good. Otherwise, he likes to grill in the backyard and watch football. His right shoulder hurts on and off and has for years. Lately, it feels sore all the time, even though he’s taken the last three months off any vigorous activity.
Is it likely he’s overtrained and overworked his shoulder muscles by spending three decades occasionally using his shoulder?
Or is it more likely that the shoulder muscles have atrophied so thoroughly from disuse that the muscles around the shoulder, ribs, and spine have become so weak, imbalanced, and poorly coordinated that he can't handle even the most rudimentary of dynamic motions?
Clearly the latter.
Over the years, I have seen many people who have had hip replacements. Do you know how many I’ve seen who had well-balanced muscles around the butt, outer thigh, anterior thigh, and inner thigh before or after the surgery?
Zero.

Model walking the catwalk with extremely weak muscles
The takeaway here is that weak, dysfunctional muscles are at the root of so many chronic joint pain complaints. Muscles facilitate movement. As organisms, we depend on them for our survival. The signals we get from muscles are predictable and helpful if we look at them carefully through the right lens.
Muscles that are unable to do their jobs—whether it's due to short-term injury, vigorous use, or chronic shortening—should and will complain.
3 Ways to Think About and Resolve Joint Pain
In summary, we've looked at the conventional orthopedic model of chronic and recurring joint pain. We've seen how thin its connection is to reality. We've seen that orthopedic theories routinely fail to explain pain and fail to explain normal human function. Here, how I think about joint pain:
Here is how I think about joint pain:
- Joint pain is often a misnomer for pain around or near the joint, and this linguistic sloppiness can mislead you into unwarranted surgeries.
- If muscles are left to atrophy or are overworked, underworked, under-stretched, or overstretched, they will (and should) tell you so!
- To fix what feels like joint pain, you should Always Think Muscles (ATM) (and of course rule out the potential ultra-rare issues like cancer and infection).
Ready to fix your own muscle imbalances? Learn to identify muscle imbalances and dysfunctions. Then learn how to fix dysfunctional muscles and muscle imbalances in this article: “How do you fix dysfunctional muscles and muscle imbalances?”
Train your mind to think right, so you can move right, so you can feel right. Set the right mental foundation for chronic pain.

